An edited version of this column, along with an accompanying table listing the market participants, was published in the January 15, 2000 issue of Ocular Surgery News.
Treatments for AMD, Even Prevention, are on the Horizon
Irving J. Arons
Managing Director
Spectrum Consulting
This year, as reported at the 1999 AAO Meeting in Orlando, for the first time it appears that one or more methods for stopping the progress of age-related macular degeneration (AMD) and, perhaps, even to improve vision for those who suffer from the disease, is on the horizon. And in an even bigger leap of faith, additional clinical work is being undertaken to determine if this terrible disease can be stopped before it progresses to the final stages that causes legal blindness.
What is AMD?
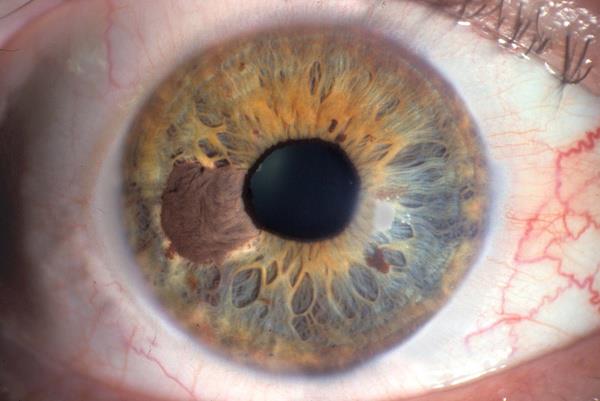
AMD is a progressive degenerative condition that damages the macula, the small central part of the retina in the back of the eye which provides central vision, and currently affects approximately 15 million people in the U.S., and at least double that in the rest of the world. Loss of central vision robs a person of the ability to perform tasks which require fine focus, such as reading, watching TV, or seeing faces. AMD can occur in two forms, the "dry" (non-exudative) form and the "wet" (exudative) form, and both can coexist in the same patient. The dry form, accounting for between 85% to 90% of AMD, is typically characterized by a build-up of drusen, white to yellow deposits underneath the retina in the macula that initially results in minimal visual symptoms. With time, vision may gradually deteriorate, depending upon drusen type, size, quantity, and location. More importantly, the presence of drusen constitutes a risk factor to develop severe vision loss due to the development of geographic atrophy or the development of the exudative (wet) form of AMD, accounting for approximately 10% to 15% of all AMD, but 90% of severe vision loss (legal blindness) in those over the age of 50.
The wet form is typically characterized by a proliferation of abnormal blood vessels (i.e., choroidal neovascularization [CNV]) underneath the macula and results in a more rapid and profound loss of central vision. About 1.5 million to 2.5 million American people (approximately 10% to 15% of all AMD cases) currently have the wet form, which accounts for the vast majority of AMD patients who are legally blind. AMD is the leading cause of blindness in the U.S. for all age groups. For persons 65 to 74 years of age, the prevalence approaches 30%. In the U.S., the current annual incidence of AMD is approximately 2 million people, 200,000 to 300,000 of whom have the wet form. It is expected that both the incidence and prevalence of AMD will increase substantially with the aging of the population.
Treatments for Wet AMD: Laser Photocoagulation
Currently, there is no clinically proven interventional therapy for dry AMD while a minority (about 15%) of patients with the wet form of AMD can be treated using laser photocoagulation, which works to close and stop progression of the bleeding CNV vessels. Photocoagulation usually causes the immediate further loss of visual acuity due to the thermal damage done to the overlying retina, and can only be applied to those patients, with "classic", well-demarcated CNV lesions. In spite of these deficiencies, laser photocoagulation is widely employed, principally because it is the only treatment option available for sufferers of wet AMD. Approximately 42,000 laser photocoagulations were performed last year, used in less than 2% of eyes with AMD. Thus there is a need for a treatment modality suitable for a large segment of AMD patients that selectively closes the choroidal neovessels with out damaging overlying neurosensory retina and without causing further loss of vision. The photodynamic therapy (PDT) approach appears to be one such treatment.
Photodynamic Therapy for Wet AMD
Most of the AMD news to date, has been on the ongoing studies of photodynamic therapy to stop the progress of classic wet AMD, those lesions that are well defined, leak heavily, and cause the most rapid deterioration of vision. Several studies are underway, with the QLT PhotoTherapuetics' team (Ciba Vision for marketing and Coherent and Carl Zeiss with the activating lasers) in the lead. QLT's PMA for Visudyne therapy recently won recommendation for approval from the FDA's Ophthalmic Drug Advisory Panel. Following behind is the Miravant team (Pharmacia & Upjohn as the marketer, and IRIDEX's Iris Medical as the laser supplier), and then Pharmacyclics (with marketing partner Alcon Laboratories, and probably Diomed as the laser supplier). FDA final approval of QLT's Visudyne injection therapy might be in hand before this article reaches print, most likely in the first quarter of 2000. Miravant's Photopoint therapy has completed enrollment of patients in its Phase III clinical trial, with a PMA expected to be filed sometime in 2000 or 2001. Pharmacyclics' Optrin therapy is even further behind, still running Phase I/II clinical trials. (Others in preclinical trials include Nippon Chemical and Toyo Kogyo, in association with Lederle Japan.) (See the table below for a listing of the players and the drugs/lasers involved.)
In the PDT approach, a photosensitizer is administered intravenously, which selectively accumulates in the neovascularized tissue. A dose of carefully calculated laser light is administered directly to the lesions, which activates the photosensitizer causing death to the cells and destroying the vessels. It is important to note that the effect of PDT treatment is photochemical and there is no accompanying thermal reactions. Although the results are a stoppage of blood leakage from the disruption of the vessels, according to the results seen in the TAP study (Treatment of Age-Related Macular Degeneration with Photodynamic Therapy), as reported at the Vitreoretinal Update '99 meeting held just prior to the AAO, the effect appears to be temporary, and as many as four treatments per year may be needed. However, there are indications that the recurrance of bleeding should lessen with time. The problem is the cost of the treatment. Visudyne is expected to be priced at about $1200 per dose, and with the surgeon and facility fee added in, a single treatment could cost as much as $2000, or $8000 per year. But, the results of the TAP study indicate that visual acuity, contrast sensitivity, and angiographic outcomes are better in verteporfin-treated eyes, than those receiving a placebo. Verteporfin therapy can safely reduce the risk of vision loss in eyes with predominantly classic CNV lesions. However, vertoporfin therapy does not appear effective for occult CNV, typically poorly defined and diffuse lesions with less leakage, the most common form, which accounts for over 70% of all "wet" AMD. In anecdotal information picked up at the AAO meeting, even though the cost appears high, most of the retinal surgeons we spoke with, expect to use the PDT approach with most of their wet AMD patients, rather than laser photocoagulation.
Newer Laser Treatments for Wet AMD
However, there are several emerging new laser treatments for AMD currently undergoing clinical trials. A few are for the treatment of wet AMD, and at least two for the prophylactic treatments of patients with high-risk drusen in the pre-neovascularization stage of dry AMD, to prevent or delay CNV.
One prospective randomized, placebo-controlled, multicenter clinical trial underway to treat wet AMD patients with subfoveal occult choroidal neovascular membranes (CNVM) with a low intensity laser is the "Transpupillary Thermotherapy for Choroidal Neovascularization" (The TTT4CNV Clinical Trial), sponsored by IRIDEX. This study uses the Iris Medical OcuLight Slx 810 nm diode laser in its unique long-pulse/large-spot size mode, known as "Transpupillary Thermotherapy (TTT), to close the CNVM without collateral damage to the overlying central retina. The laser is used to induce localized hyperthermia, but below the coagulative threshold, to close the choroidal vessels. In a recently published study Elias Reichel, MD of The New England Eye Center (Boston) noted that in a small sample of eyes (16 eyes of 15 patients), 75% of TTT patients experienced improved or stable visual acuity post therapy. Another small study, presented at this year's AAO meeting by Richard Newsome, MD, performed at the King's College Hospital in London, UK, showed that after an average of 6.5 months follow-up after the TTT treatment, the CNV resolved in 71% of treated eyes and visual acuity stabilized in 86% of treated eyes.
Iridex is also involved in a second laser photocoagulation study for the indirect closure of subfoveal occult or classic CNVM through the laser treatment of the extrafoveal feeder vessels. This treatment, uses dynamic high-speed indocyanine green (ICG) dye-enhanced angiography to identify and localize the tiny feeder vessels, and the same OcuLight Slx 810 nm diode laser, to treat them with a train of repetitive infrared laser pulses. In an initial study, reported by Bert Glaser, MD, at the Vitreoretinal Update meeting preceding the AAO, over 80% of the feeder vessels treated were closed one day following treatment, with the patients noting a subjective improvement in vision and minimal side effects. The company is in the process of considering undertaking a multi-center study of this procedure.
Laser Therapy for Dry AMD
But, perhaps even more exciting than the studies underway to treat wet AMD, are the two studies being undertaken by IRIDEX and the one by the National Eye Institute (NEI) to prophylactically treat patients at risk with drusen secondary to dry AMD. The idea is to attack the disease much earlier in its course to reduce drusen, stabilize of improve vision and possibly prevent or delay the progression to the exudative form. The first is a therapeutic treatment to reduce drusen for vision improvement. An article in the November issue of Ophthalmology, entitled "Therapeutic Benefits of Infrared (810 nm) Diode Laser Macular Grid Photocoagulation in Prophylactic Treatment of Nonexudative Age-Related Macular Degeneration", by Joseph Olk, MD, of the Retina Center of St. Louis, et al, discusses the 2-year clinical pilot trial in detail. The findings showed evidence that laser therapy resolved the drusen and improved vision. This study used both visible laser burns and subthreshold (invisible) laser treatments to determine if the effects on the reduction/elimination of drusen would improve/stabilize visual acuity and reduce/delay the incidence of CNV. Results of the pilot study showed resorption of drusen in 68% of treated eyes and visual acuity improvement in 24% of a subset of treated eyes after a single treatment. One purpose of the pilot study was to determine the appropriate laser dose to be used in a follow-up prophylactic study, described below. (There is some evidence that the therapeutic approach is effective, while there is no evidence yet that the prophylactic approach is effective.)
The second IRIDEX-sponsored trial, the "Prophylactic Treatment of Age-Related Macular Degeneration" (PTAMD) trial, following up on the results obtained with the subthreshold treatments done in the study above, is designed to more definitively evaluate the prophylactic treatment of high-risk drusen-evident patients using minimal, gentle, subthreshold micropulse 810 nm laser treatments placed in a grid surrounding the drusen, to halt or delay progression from the dry form of AMD to the wet form. The PTAMD trial is currently in its second year, with over 400 patients participating, of an anticipated 1000 to 1300 to be enrolled. Study results are anticipated in about three years.
And the NEI-sponsored study, called "Complications of Age-Related Macular Degeneration Prevention Trial" (CAPT), is to determine if low intensity argon laser treatment prophylactically decreases vision loss for people at risk for severe AMD. Twenty-four selected sites across the country are participating in the CAPT trial. It is designed to assess the safety and effectiveness of low intensity laser light to prevent disease progression and loss of vision in people who are at risk for severe AMD. The CAPT study will enroll a total of 1000 patients at 24 clinical centers across the United States during an 18-month period. The trial is expected to last at least five years.
Unanswered Questions
An important question, yet to be answered, is who will do the needed diagnosis to determine who is eligible for treatment to prevent this disease. In today's managed care environment, the retinal specialist who has the laser and diagnostic tools to treat the early stages of the disease rarely sees the patients at risk. They are usually seen by the general ophthalmologist. Will he/she be motivated to look for the very early signs of AMD to get his/her patients into a prophylactic or early treatment program. Perhaps, as the word is spread that such treatments are available, and with the advent of the internet, a more educated consumer/patient will know to ask the right questions, and to demand the appropriate treatments. Only time will tell, but the next few years will be very interesting in the diagnosis and treatment of AMD.